Researchers are taking on the myth that eating disorders only affect women by training general practitioners to spot symptoms in men and offer better, stigma-free care.
 Study: Intervention against the stigmatization of men with eating disorders in primary care (iSMEsH): Protocol for a randomized mixed-methods evaluation trial. Image credit: F01 PHOTO/Shutterstock.com
Study: Intervention against the stigmatization of men with eating disorders in primary care (iSMEsH): Protocol for a randomized mixed-methods evaluation trial. Image credit: F01 PHOTO/Shutterstock.com
A recent PLoS One study discussed an intervention against the stigmatization of men with eating disorders in primary care (iSMEsH) to reduce stigma over eating disorders (EDs) in men, to spread awareness among German general practitioners (GPs), and challenge the perception that EDs are “women’s diseases”.
Eating disorders in men and stigmatization
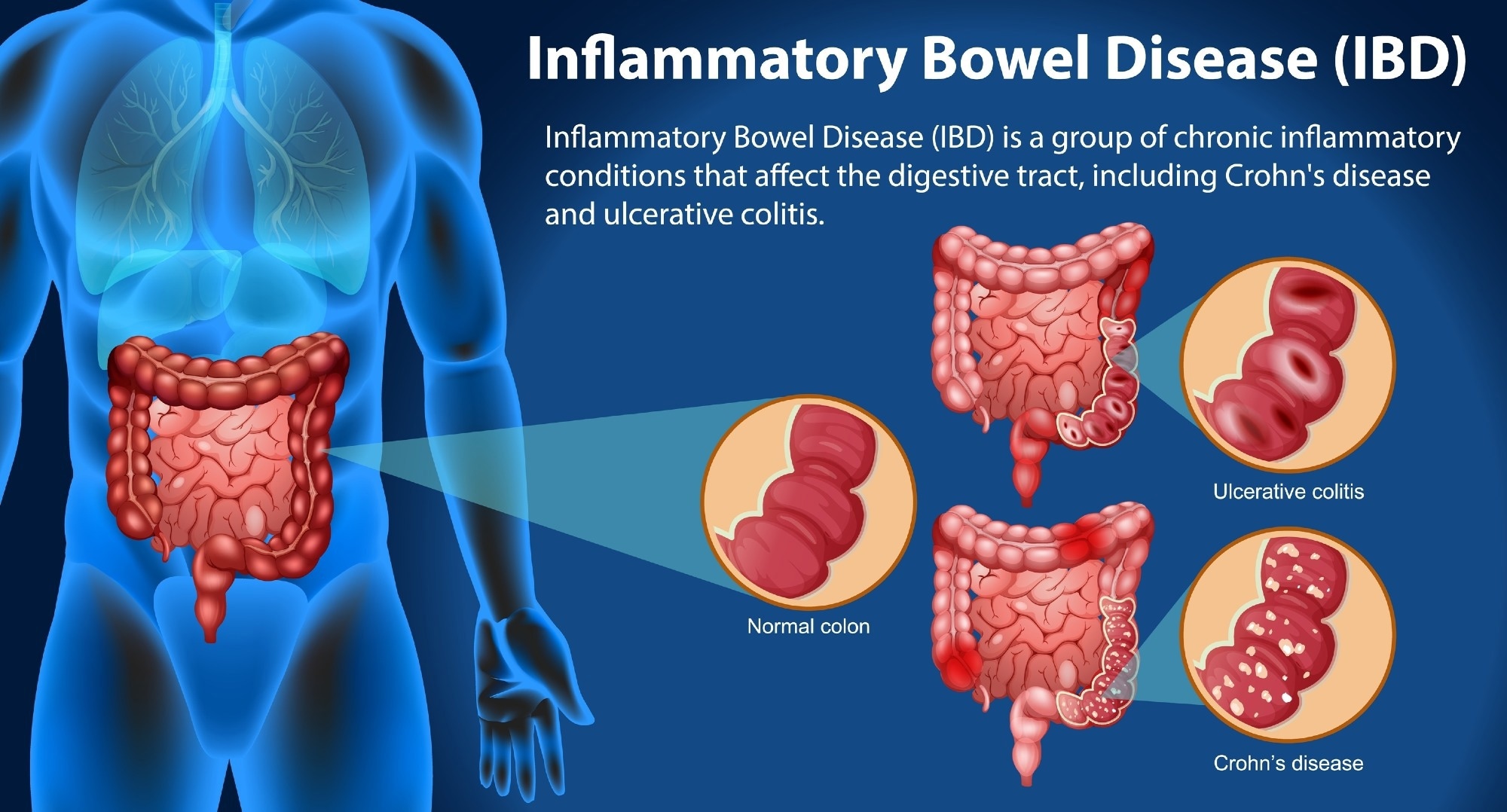
The most common forms of EDs are Bulimia nervosa, Binge-eating disorder, and Anorexia nervosa. Individuals with ED report a notably higher mortality risk compared to the general population. The treatment costs are also substantial because of the frequent occurrence in adolescence, the lengthy duration of treatment, and repeated inpatient stays.
Some estimates suggest that men account for one in every four cases of ED; however, they remain underrepresented in ED research and care. A significant reason for this underrepresentation could be the stigma attached to EDs, which are broadly considered as “women’s diseases” and seen as conflicting with traditional masculine identity norms. Such self-stigmatization prevents men from disclosing ED symptoms and seeking help. Even for medical professionals, the stereotype of ED as “women’s diseases” shapes their views. Therefore, the question of how to address stigmatization and stereotypes among medical professionals regarding men with EDs remains unresolved.
Study aims and sample selection
This study aims to raise awareness of the issue of EDs among men and sensitize GPs in primary care in Germany to the manifestation of EDs in men. An intervention on EDs in boys and men for doctors is being developed, disseminated, and evaluated as part of this effort.
The study follows a sequential mixed-methods design, including pre-implementation focus groups and panel discussions, a randomized controlled online training phase, and post-implementation qualitative interviews. The operating hypothesis is that participation in the intervention will lead to individual decreases in stigmatizing attitudes and increases in knowledge and self-efficacy.
Study participants will be recruited nationwide, including adult males with lived experience of EDs, GPs, and medical students. Men with lived experience of an ED will participate in the pre-implementation phase, contributing to the development and refinement of the intervention rather than the randomization trial itself. Participants with lived experience of an ED were adult males willing to provide written informed consent and had received a current or past ED diagnosis. The focus group will include GPs regularly treating men in their healthcare institution.
Eligible participants will be randomized to a wait-list control group (i.e., 14-day delay before online training access) or the intervention group (i.e., immediate access to the self-paced online training period) in a 1:1 ratio. Six short, separate modules will be presented for online completion in 5–10 minutes each, followed by interactive questions, quizzes, and ratings. The total duration of the training is 45-50 minutes.
The primary outcomes include the cognitive, behavioral, affective, and facets of ED-associated stigma and a range of implementation outcomes based on the Implementation Outcomes Framework, such as acceptability, feasibility, appropriateness, and adoption.
The secondary outcome will include stigma-related perceptions of EDs in men. A sample size of 74 participants is needed to achieve the best results, i.e., a minimum of 37 participants per group. The study aims to include an experimental group of approximately 50 GPs and a control group of another 50 GPs. In addition, around 50 medical students in their clinical training year will also complete the training to explore its educational relevance. Recruitment and data collection started on July 23, 2024, and are expected to be completed by November 1, 2025. The results are expected by the end of 2025.
Data collection, analysis, and monitoring
Participant data will be collected pseudonymously via electronic data capture tools. The cognitive facet of stigma will be assessed in terms of knowledge deficits regarding EDs in men and boys. A modified version of the German Opening Minds Stigma Scale for Health Care Providers (OMS-HC) will be used to gauge the affective facet of stigma. An adapted version of the General Self-Efficacy Scale (GSE) will be used to assess the behavioral facet of stigma. Baseline variables, such as gender role endorsement, will also be evaluated using the Traditional Masculinity-Femininity Scale (TMF). Data will be collected on sociodemographic features, including age, sexual orientation, gender, and others.
Quantitative data management will be handled using the Moodle learning management system and jsPsych survey tools. At the same time, qualitative data (from interviews and focus groups) will be transcribed and analyzed using MAXQDA. Audio recordings will be used to collect qualitative data. Personal and outcome data will be stored separately and assessed for plausibility, completeness, quality, and range validation. Quantitative data analyses will be performed using R and SPSS in two sets: per-protocol and intention-to-treat analyses. Qualitative data will be analyzed thematically following the Braun and Clarke (2006) framework.
The study does not include experimental manipulations, so there will not be a data monitoring committee. The participants can contact the principal investigator anytime, and participation is entirely voluntary. The adverse events are likely to be addressed on a case-by-case basis in collaboration with the relevant participants, and these events will be documented in scientific publications.
Conclusions
The iSMEsH intervention aims to sensitize German primary care to the manifestation and occurrence of EDs in men, impart necessary skills, and combat the stigmatization that EDs are “women’s diseases”.
The main strength of this intervention revolves around its comprehensive nature, targeting different facets of stigmatization. The involvement of participants with lived experience guarantees that the intervention aligns with the requirements of those most affected. By engaging GPs and medical students, the project also seeks to embed awareness and anti-stigma education at multiple professional levels.
The main limitation of this study is that it will not assess the long-term implementation outcomes. Additionally, the findings cannot be generalized due to the utilization of self-reported data and the narrow focus on the German healthcare system.
Journal reference:
- Lehe MS, et al. (2025). Intervention against the stigmatization of men with eating disorders in primary care (iSMEsH): Protocol for a randomized mixed-methods evaluation trial. PLOS ONE, 20(10), e0333997. https://doi.org/10.1371/journal.pone.0333997. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0333997
.jpeg)





















.jpeg)













 English (US) ·
English (US) ·