Home / Featured Content / Empowering Pharmacists Is About More Than Saving Emergency Departments – It’s About Equity in Health Care
At the time, the government framed this as a way to reduce strain on family physicians and over-crowded emergency departments (EDs).
October 11, 2025 by Healthy Debate Leave a Comment

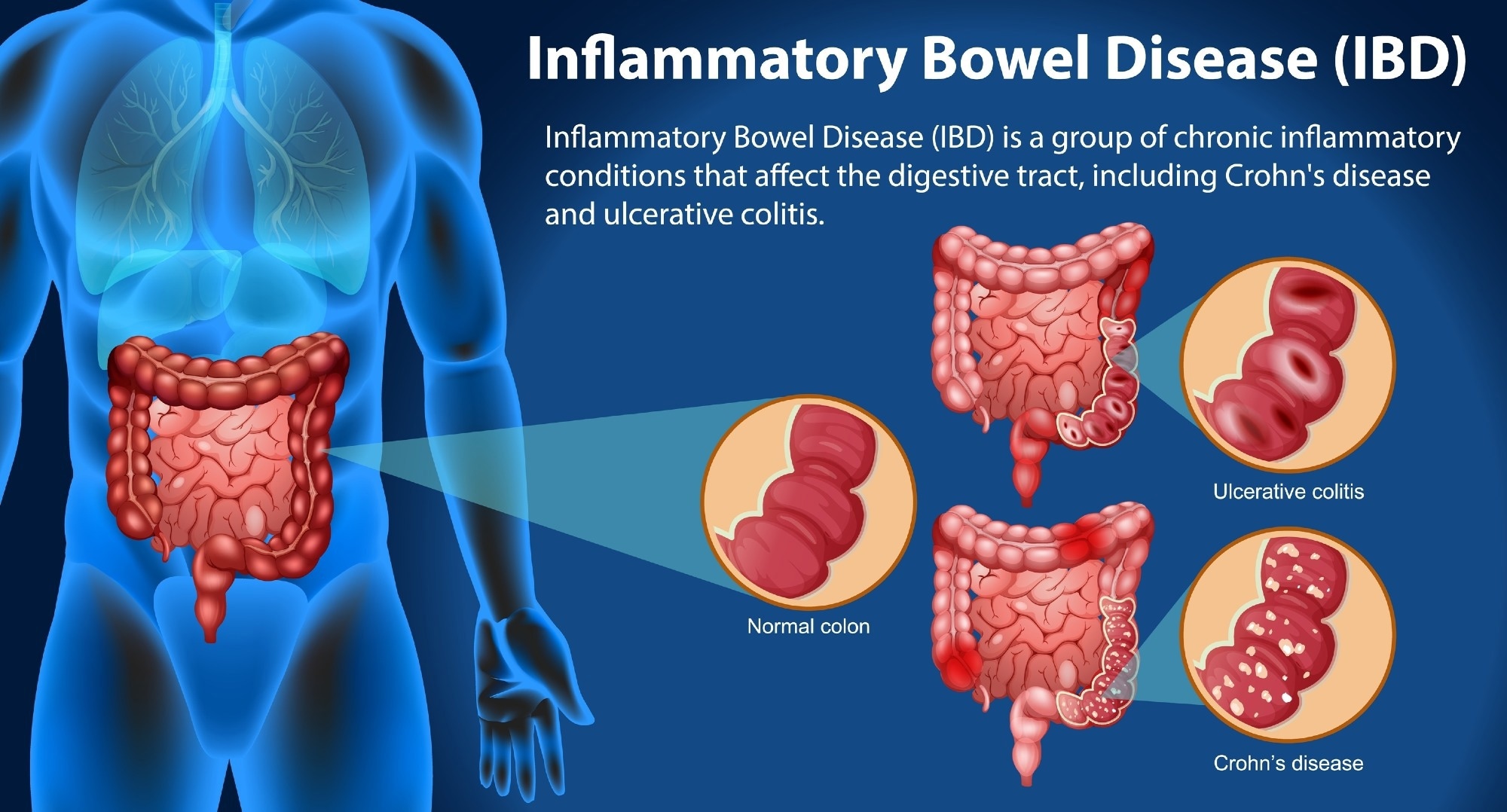
In January 2023, Ontario gave pharmacists the authority to prescribe for 13 minor ailments such as urinary tract infections, pink eye, dermatitis and seasonal allergies. Pharmacist prescribing was expanded again in October 2023 and new policy proposals are considering expanding that scope further, including prescriptions for the common cold, fungal infections and dandruff.
At the time, the government framed this as a way to reduce strain on family physicians and over-crowded emergency departments (EDs). On the other hand, physician labour groups like the Ontario Medical Association argued that shifting prescribing to pharmacists might mean lower-quality care with a tendency to over-prescribe.
New evidence from our team suggests that not only did the reform reduce ED strain while increasing demand for outpatient physician care, but it also has done something neither side imagined: reduce inequities in access to care.
Our recent study used anonymized mobility data to track how this policy caused shifts in patients’ health-care seeking behaviour. We found three key results:
- The policy generated pharmacy traffic: Immediately after the policy was enacted, pharmacy visits rose by about 16 per cent; this persisted throughout the first year of the policy.
- Pharmacy visits are more accessible for some marginalized populations: Those from lower-income communities or neighbourhoods facing higher levels of material deprivation saw the largest increases in pharmacy use post-policy.
- Pharmacy visits relieved ED visits while preserving outpatient care. We observed that ED foot traffic fell by 9 per cent while visits to outpatient physicians rose by 4 per cent. This implies that visiting a pharmacist for health care doesn’t reduce physician visits or potentially endanger patients but can meaningfully free up ED space for more serious cases.
However, there was a caveat in our findings: while those in low-income communities were able to access higher levels of care through pharmacies, those living in immigrant and visible minority populations did not enjoy the same benefits. This raises concerns about uneven uptake.
For many Ontarians, especially those without a regular family physician, pharmacists are the most accessible health professional in their community
For many Ontarians, especially those without a regular family physician, pharmacists are the most accessible health professional in their community. They’re more geographically dispersed, typically open evenings and weekends, and don’t require appointments. It’s much easier to get a pharmacist on the phone, for example, than even your own family physician.
Hence, making care for low-acuity health events accessible through pharmacies can translate into real boosts in accessing care, particularly for people living in low-income neighbourhoods. Our findings show that scope-of-practice reform isn’t just about convenience: it can rebalance access in ways that bring care closer to some individuals who often struggle to get it.
And these benefits don’t have to come at the expense of worse patient care. We find that pharmacists may provide a critical stopgap for ED use, but they don’t substitute for outpatient care at a physician’s office. If anything, visits to pharmacies and clinics are complementary, particularly for the most vulnerable patient groups.
Still, equity does not expand automatically. We observed limited success among immigrant and minority populations. This suggests that barriers – whether due to language, institutional mistrust or something else – may be critical to overcome to ensure access barriers are universally reduced.
There are also risks of overuse of prescriptions or fragmented care. Pharmacist prescribing will be the most beneficial for patients when pharmacists and primary care providers are well-integrated so patients don’t fall through the cracks. And pharmacists may still have financial incentives to write prescriptions, even when it is not the best for the patient.
Based on the evidence, we see four clear priorities for policymakers and health leaders:
- Prioritize awareness and outreach. Public campaigns should capitalize on these policies’ potential to reduce disparities in access. These campaigns should be multilingual and culturally sensitive to increase their reach to other vulnerable communities.
- Integrate pharmacists into primary care teams. Communication systems should be built to allow pharmacists to share prescribing records with family physicians and other primary care professionals.
- Expand scope cautiously but ambitiously. Adding more conditions may be beneficial, particularly in rural and underserved areas where access gaps are greatest.
- Evaluate outcomes beyond utilization. Future research should measure patient outcomes, satisfaction and cost-effectiveness to ensure benefits are not just theoretical.
Allowing pharmacists to prescribe in Ontario may prove to be a valuable pressure relief for family physicians and EDs. But to ensure the benefits reach everyone, especially immigrant and minority communities, we need policy that integrates pharmacists into primary care and is dedicated to reaching all patient groups.
In that sense, expanding pharmacists’ role in primary care may be the beginning – not the end – of a broader restructuring ensuring all patients can access primary care.
—
Previously Published on healthydebate.ca with Creative Commons License
***
–
The world is changing fast. We help you keep up.
We’ll send you 1 post, 3x per week.
Join The Good Men Project as a Premium Member today.
All Premium Members get to view The Good Men Project with NO ADS. Need more info? A complete list of benefits is here.
—
Photo credit: iStock
About Healthy Debate
Healthy Debate publishes journalism about health care in Canada by the people whose lives it touches the most, from physicians, patients and caregivers to health journalists, academics, and advocates. Our unique focus on giving a platform to health-care insiders allows us to provide detailed coverage of the inner workings—and dysfunctions—of this important sphere of Canadian society.
We pride ourselves on covering the nitty gritty of Canadian health care through clear, captivating op-eds and reported features. This allows us to be a forum where the general public learns about, discusses, and debates health care in Canada—and, importantly, imagines what it could become.
Visit the website at https://healthydebate.ca/. On Twitter: @healthydebate
.jpeg)























.jpeg)












 English (US) ·
English (US) ·